![]()
Post myocardial infarction depression, prevalence, diagnosis, pathophysiologic mechanisms, treatment and management
Year: 2024; Volume: 4; Issue: 3; Page No: 15 – 21
Article Type: Short Communication
Authors: Bayan Omar Sharif *1![]() , Nazdar Qudrat Abas 2, Peshin Abdalstar Salih3, Talar Jamal Rahim4, Shahla Hamid Hassan5
, Nazdar Qudrat Abas 2, Peshin Abdalstar Salih3, Talar Jamal Rahim4, Shahla Hamid Hassan5
![]() https://doi.org/10.55349/ijmsnr.2024431521
https://doi.org/10.55349/ijmsnr.2024431521
Affiliations: *1Health Development and Training Center, Sulaimani Directorate of Health, Sulaimani, Kurdistan Region, Iraq. Email ID: omerbayn82@gmail.com
2Department of Psychology, College of Education, University of Garmian. Email ID: nazdar.qudrat@garmian.edu.krd
3The British International School of Sulaymani. Iraq, Email ID: peshinsaleh@gmail.com
4Sulaimani Directorate of Health, Sulaimani, Kurdistan Region, Iraq, Sulaimani Burn & Plastic Surgery Hospital. Email ID: talar.138193@gmail.com
5Sulaimani Directorate of Health, Kurdistan Region, Iraq, Soz mental hospital. Email ID: shahlahamid81@gmail.com
Corresponding Author:
Dr. Bayan Omar Sharif, M.Sc. (N), Ph.D.,
Health Development and Training Center,
Sulaimani Directorate of Health,
Sulaimani,
Kurdistan Region,
Iraq.
Email ID: omerbayn82@gmail.com
| How to cite this article: Sharif OB, Abas NQ, Salih PA, Rahim TJ, Hassan SH. Post myocardial infarction depression, prevalence, diagnosis, pathophysiologic mechanisms, treatment and management. Int J Med Sci and Nurs Res 2024;4(3):15–21 DOI: 10.55349/ijmsnr.2024431521 |
Article Summary: Submitted: 10-July-2024 Revised: 30-July-2024 Accepted: 21-August-2024 Published: 30-September -2024
Abstract
Background: Myocardial infarction (MI) can have significant physical and mental consequences. Depression is a prevalent psychiatric condition after MI which can reduce the quality of life and increase the mortality rates of patients. The link between depression and poor cardiac outcomes has prompted clinical trials investigating the impact of treating depression on both outcomes.
Methods: In this paper, we discussed about post Myocardial infarction depression, its Prevalence, pathophysiologic mechanisms, such as neurobiological mechanisms of post-MI depression, Hypothalamic-pituitary-adrenal axis and autonomic nervous system, environmental factors, like lack of social support, lifestyle changes, economic status and health related anxiety.
Results: By 2030, depressive disorders are projected to become the first leading cause of disease burden in high-income countries and the second leading cause globally. Depression is prospectively linked to negative cardiac outcomes, regardless of other cardiovascular risk factors. In individuals who are initially healthy, depression is correlated with a greater likelihood of developing heart disease compared to those without depression.
Conclusion: We have concluded that several factors including the dysregulation of the autonomic nervous system and Hypothalamic-pituitary-adrenal axis, various environmental factors, and genetics can be contributed to the correlation between Myocardial infarction and depression.
Keywords: Post myocardial infarction, depression, prevalence, diagnosis, pathophysiologic mechanisms, treatment, management
Full Text
Introduction
Depression in patients with cardiovascular disease is independently associated with progression of heart disease, major adverse cardiac events, and mortality. [1] Depression is a highly prevalent mental health disorder that exerts considerable economic and social burdens. [2] It is estimated that over 300 million individuals worldwide (4.4%) are affected by depression, with higher prevalence rates among females (5.1%) compared to males (3.6%). Furthermore, the incidence of depressive disorders tends to increase with age, impacting over 7.5% of females and 5.5% of males aged over 55 years. [3] Projections indicate that by 2030, depressive disorders are expected to emerge as the leading cause of disease burden in high-income countries and the second leading cause globally. [4]
Myocardial infarction (MI), recognized as the most severe form of ischemic heart disease (IHD), can lead to numerous physical and mental health challenges. Depression is one of the most common psychological responses following MI. [5] A recent meta-analysis involving over 12,000 MI patients revealed that approximately 29% experienced depression. [6] This post-MI depression can adversely affect quality of life and increase patient mortality. [7] Additionally, it is associated with a 2 to 2.5-fold heightened risk of cardiovascular complications. [8] In this brief communication, we aim to explore post-MI depression and its underlying pathophysiological mechanisms in patients with cardiac disease.
Materials and Methods
Prevalence of post MI depression
Heart disease accounts for over 30% of annual deaths globally. [9] Among individuals with coronary artery disease (CAD), depression is prevalent, with approximately 30% exhibiting elevated depressive symptoms, and 15% to 20% fulfilling the criteria for major depressive disorder. [10] This prevalence is 2 to 3 times greater than that observed in the general population. Similarly, the incidence of depression is notably high among patients with heart failure. [11]
Depression is prospectively linked to adverse cardiac outcomes, independent of other cardiovascular risk factors. In initially healthy individuals, depression is associated with a higher incidence of new-onset heart disease compared to those without depression. [12] Among individuals with pre-existing cardiac conditions such as coronary artery disease [13], recent acute coronary syndrome [14], and those who have undergone coronary artery bypass graft surgery [15], depression is independently correlated with elevated rates of recurrent events and mortality. Given the extensive evidence connecting depression to negative outcomes in patients with acute coronary syndrome (ACS), the American Heart Association has recognized depression as an independent risk factor for poor prognosis following ACS. [14] Similarly, depressed patients with heart failure (HF) experience increased healthcare utilization, more frequent hospitalizations, and higher mortality rates, regardless of HF severity. [11] Additionally, depression is associated with a higher recurrence of atrial fibrillation. [16]
Furthermore, depressive symptoms are frequently chronic and recurrent among patients with heart disease, with those experiencing untreated or inadequately treated depression being at a higher risk for adverse outcomes, including increased mortality. [17] Conversely, some observational studies suggest that treating depression is associated with improved outcomes and reduced rates of cardiovascular mortality. [18] The mechanisms linking depression to negative cardiac outcomes are likely multifactorial, encompassing both physiological and behavioral factors. [19] The prevalence of depression and its influence on prognosis in individuals with cardiovascular disease (CVD) underscore the potential benefits of effectively treating depression to enhance quality of life and possibly prevent adverse cardiac outcomes. While the association between depression and heart disease is well established, significant practical questions remain regarding the safe and effective management of depression in this population. Various strategies have been employed to address depression in patients with heart disease; however, the evidence regarding the efficacy and clinical impact of these approaches on both psychiatric symptoms and cardiac-related morbidity remains conflicting [20].
Pathophysiologic mechanisms of post MI depression
- Neurobiological mechanisms of post-MI depression
Despite its prevalence, post- MI depression is frequently overlooked as a mere emotional response to physical illness. Furthermore, emerging evidence indicates that depression itself is a significant risk factor for MI. This study aims to illuminate the pathways linking MI and depression by outlining potential pathophysiological mechanisms. Table-1 presented an updated, comprehensive overview of the relationship between post-MI depression and various factors, including dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system, dysfunction of the coagulation system, inflammation, and genetic factors. [21]
Table – 1 Neurobiological mechanisms of post-MI depression [21]
|
Role of the autonomic nervous system and HPA axis
|
· Continuous upregulation of the HPA and SA systems
· Activation of pro-inflammatory cytokines and the HPA and autonomic nervous systems · Emotional stress and serotonin dysregulation in depression · Hypercortisolemia |
Role of coagulation system | · ↓ levels of BDNF and tPA in emotional stress and depression
· ↑ levels of PAI-1 in depression · ↑ levels of PAI-1 lead to ↓ levels of BDNF |
Role of inflammation | · Lack of oxygen—DAMPS release—immune cells activation—pro-inflammatory cytokines—↑ release of IL-1, IL-6, TNF-α, CRP—↑ kynurenine pathway activation—↑ NMDA receptor agonists production
· Pro-inflammatory cytokines—altered neurotransmitters metabolism and production · Pro-inflammatory cytokines—↓ levels of BDNF |
Genetic correlation | · Depression linked with ↑ risk of heart failure and small vessel stroke
· Depression and CVD—↑ levels of IL-6, CRP, and triglycerides · Variant serotonin transporter gene (5-HTTLPR) ↑ risk of depression after MI, poor response to antidepressants · Variant serotonin receptor gene (5-HT2A)—↑ risk of depression after MI · IL-1 gene—↑ risk of depression after MI, pro-inflammatory response |
In Table–1, HPA, hypothalamic-pituitary-adrenal; SA, sympathetic-adrenomedullary; TNF-α: tumor necrosis factor-alpha, interleukin 6 (IL-6), interleukin 1 (IL-1), C-reactive protein (CRP), LDL, low-density lipoprotein; HDL, high-density lipoprotein; PVCs, premature ventricular contractions; GP IIb/IIIa, glycoprotein IIb/IIIa; GP Ib/IX, glycoprotein Ib/IX; BDNF, brain-derived neurotrophic factor; tPA, tissue-type plasminogen activator; PAI-1, plasminogen activator inhibitor-1; DAMPs, damage-associated molecular patterns; MI, myocardial infarction; CVD, cardiovascular disorders.
2. Hypothalamic-pituitary-adrenal axis and autonomic nervous system
Myocardial infarction triggers multiple consequential responses, including activation of the hypothalamic-pituitary-adrenal (HPA) axis and dysregulation of the autonomic nervous system. These effects, illustrated in Figure–1, may lead to selective dysfunction in the prefrontal cortex and anterior cingulate gyrus, which can contribute to the development of depression. [22]
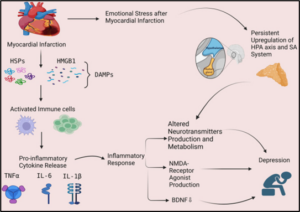
Figure-1 showed the possible role of inflammatory response and hypothalamic pituitary axis as possible mechanisms in post-MI depression. Myocardial infarction leads to a lack of oxygen and the release of damage-associated molecular patterns (DAMPs), such as high-mobility group box 1 (HMGB1) and heat shock proteins (HSPs). These DAMPs activate immune cells, such as macrophages, which phagocytose the damaged tissue and release pro-inflammatory cytokines, such as interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), leading to an inflammatory response. Inflammation can lead to depression through 3 mechanisms including: (1) altering the production and metabolism of neurotransmitters, (2) increased production of N-methyl-D-aspartate (NMDA) receptor agonist and, (3) decreased levels of brain-derived neurotrophic factor (BDNF). Myocardial Infarction also cause emotional stress which activates the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic-adrenomedullary (SA) system and can cause altered metabolism and production of neurotransmitters, leading to depression. HPA, hypothalamic-pituitary-adrenal; SA, sympathetic-adrenomedullary; DAMPs, damage-associated molecular patterns; HMGB1, high-mobility group box-1; HSPs, heat shock proteins, TNF-α, tumor necrosis factor-alpha, interleukin 6 (IL-6), Interleukin 1β (IL-1β), NMDA, N-methyl-D-aspartate; BDNF, brain-derived neurotrophic factor.
A recent study on post- MI patients found an immediate increase in cortisol levels due to the activation of the HPA following MI, which returned to baseline within 72 hours. No significant differences were observed between morning and afternoon cortisol levels in individuals with post-MI depression. However, patients experiencing depression for more than three months exhibited a markedly flattened daily cortisol secretion rhythm. In contrast, post-MI patients without depression showed significantly lower afternoon cortisol levels compared to morning levels. Abnormalities in cortisol rhythm have been associated with cognitive impairment and diminished stress-coping capabilities, potentially heightening the risk of depressive symptomatology. [22] Additionally, emotional stress related to post-MI depression can activate the sympathetic-adrenomedullary system, which, together with HPA axis activation, may lead to serotonin dysregulation and contribute to the persistence of depressive symptoms. [23]
3. Environmental factors
Various lifestyle and environmental factors have been recognized as potential contributors to the onset of post-MI depression. These include inadequate social support, challenges in implementing lifestyle changes, financial stress, and health-related fears and anxiety. [24]
3.1. Lack of social support
A deficiency in social support or an inadequate support system has been associated with a heightened risk of post-myocardial infarction (MI) depression. Insufficient emotional or practical assistance from family, friends, or healthcare providers can intensify feelings of isolation, sadness, and distress. Conversely, robust social support can enhance individuals’ ability to cope with the emotional difficulties encountered after an MI. [25]
3.2. Lifestyle changes
Post-myocardial infarction (MI), patients are frequently encouraged to undertake substantial lifestyle changes, including adopting a nutritious diet, participating in regular exercise, ceasing smoking, and minimizing alcohol intake. Challenges in initiating and sustaining these lifestyle modifications, coupled with the persistence of unhealthy habits such as physical inactivity, poor dietary practices, smoking, and excessive alcohol consumption, are linked to an increased risk of post-MI depression. These detrimental behaviors can not only exacerbate physical health outcomes but also impair mood regulation and foster a negative emotional state. [26]
3.3. Financial stress
Financial stress stemming from medical costs, income loss, or the inability to work following a MI can significantly contribute to the onset of post-MI depression. Such financial challenges often exacerbate feelings of anxiety, worry, and uncertainty about future stability, thereby adversely affecting mental health and overall well-being. [24]
3.4. Health-related anxiety
Following a myocardial infarction (MI), individuals often experience health-related anxiety characterized by concerns about recurrent cardiac events, apprehension regarding physical activity, and hypochondriacal tendencies. Such anxieties can exacerbate emotional distress, promote avoidance of exercise, and diminish overall quality of life, which may, in turn, facilitate the onset of depression. [27] Furthermore, various additional factors can intensify these environmental influences and play a significant role in the emergence of post-MI depression. Noteworthy among these are pre-existing mental health disorders, particularly a history of anxiety or depression, as well as complications encountered during hospitalization. [28]
4. Genetic factors
Recent Mendelian randomization (MR) studies have revealed a significant link between genetic predisposition to depression and an increased risk of cardiovascular disease (CVD) and myocardial infarction (MI). Depression driven by genetic factors also elevates the likelihood of heart failure and small-vessel stroke, with long-term effects on MI risk. [29] Both genetic and environmental influences contribute to the development of depression after MI. For instance, a variant of the serotonin transporter gene (5-HTTLPR) has been associated with a higher risk of post-MI depression, as well as poorer responses to antidepressants. [30] Additionally, patients with a family history of depression or those experiencing high stress during an MI are at greater risk of developing depression post-MI. A review by [31] suggested that the elevated risk of thromboembolic events in individuals with depression and CVD may be linked to the increased sensitivity of serotonin receptors (5-HT2A/1B) and decreased function of serotonin transporter (5-HTT) receptors. The S allele of the 5-HTT gene has been correlated with depressive symptoms and cardiac events. Although these findings point to a genetic role in post-MI depression, the disorder is multifaceted, necessitating further research to fully explore its genetic mechanisms and potential therapeutic targets. [32]
Figure–2 Biological Mechanisms and Behavioral Mediators Linking Depression and Cardiovascular Disease [33]
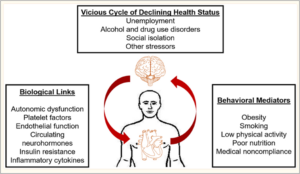
5. Biological Links between Depression and Cardiovascular Disease
Various biological mechanisms have been suggested to account for the poor prognosis in patients with cardiovascular disease (CVD) and depression. These mechanisms include lifestyle factors, autonomic dysfunction, neuroendocrine dysregulation, inflammation, insulin resistance, and heightened platelet reactivity Figure–2. Notably, these systems exhibit significant functional overlap and interaction in the regulation of both cardiac and neuropsychiatric processes [33].
Diagnosis and treatment of post MI depression
Depression is frequently undiagnosed and untreated among individuals with cardiovascular disease. Research indicates that fewer than 25% of cardiac patients with major depression receive a diagnosis, and only about half of those diagnosed receive appropriate treatment. Several factors contribute to this issue: (a). The overlap of symptoms such as fatigue and insomnia between depression and heart disease; (b). The misconception among both patients and healthcare providers that depression is a normal reaction to heart conditions; (c). Patients’ reluctance to disclose depressive symptoms; (d). Physicians’ hesitancy to inquire about depression, and (e). Concerns regarding the potential side effects of prescribing antidepressants in cardiovascular patients. [34]
Management of post MI depression
Psychosocial Treatment (non–pharmacological treatment)
Cognitive-behavioral therapy (CBT) is the most effective psychosocial treatment for depression following a myocardial infarction. It emphasizes active patient participation and focuses on five key elements: environment, thoughts, emotions, behavior, and physiology. CBT encourages patients to modify controllable stressors in their environment. Physicians can address both valid and erroneous beliefs about post-myocardial infarction care, such as the fear that physical activity may lead to sudden death. By correcting these misconceptions, they can improve treatment adherence and foster a positive outlook. Encouraging reasonable participation in exercise, hobbies, and cardiac rehabilitation, as well as teaching relaxation techniques, can help reduce anxiety. Involving family members in the rehabilitation process is crucial, as they often share similar feelings of helplessness and depression. Educating families and providing resources can enhance their supportive role in recovery. [1]
Pharmacologic Treatment
When choosing a pharmacological treatment for depression following myocardial infarction, both efficacy and adverse effects are critical factors. Generally, there is minimal difference in the effectiveness of antidepressants for mild to moderate depression; however, their side effect profiles vary significantly. The cardiac implications of frequently prescribed antidepressants are noteworthy. Over the past twenty years, selective serotonin reuptake inhibitors (SSRIs) have become the primary choice for treating mild moderate depression. Unlike tricyclic antidepressants (TCAs), SSRIs have been shown to be safe and exert minimal influence on cardiovascular function, even in overdose scenarios. They do not affect fast sodium channels or conduction pathways and lack proarrhythmic or antiarrhythmic properties. A comparative study demonstrated that the discontinuation rate due to cardiovascular events was substantially higher in patients taking nortriptyline, a relatively tolerable TCA with low cholinergic activity, compared to those on paroxetine (7 out of 40 vs. 1 out of 41). Furthermore, the study indicated a statistically significant rise in pulse rates both in supine and standing positions among subjects receiving nortriptyline. [35]
Conclusion
Several factors contribute to the correlation between myocardial infarction and depression, including dysregulation of the autonomic nervous system, the hypothalamic-pituitary-adrenal axis, various environmental influences, and genetic factors. The co-occurrence of these conditions can significantly affect the quality of life for individuals impacted by both. Depression and cardiovascular diseases share numerous biological mechanisms and behavioral mediators, as indicated by the bidirectional arrows, which illustrate the vicious cycle of deteriorating health outcomes that may arise from depression in patients with cardiovascular disease, exacerbated by negative lifestyle and socioeconomic factors. The prevalence of depression and its influence on prognosis in individuals with cardiovascular disease (CVD) underscore the potential benefits of effectively treating depression to enhance quality of life and possibly prevent adverse cardiac outcomes. Notably, depression often goes undiagnosed and untreated in this population. Several studies have investigated the efficacy of psychotherapy for treating depression in heart disease patients, with cognitive behavioral therapy (CBT) being the most extensively researched. When considering pharmacological treatments for depression following myocardial infarction, careful selection is crucial.
Source of funding: None
Conflict of Interest: Nothing to declared by the authors
Authors’ Contributions: All authors conceived and designed the article. Wrote the full paper and checked by all the authors.
References
- Zambrano J, Celano CM, Januzzi JL, Massey CN, Chung WJ, Millstein RA, et al., Psychiatric and psychological interventions for depression in patients with heart disease: a scoping review. Journal of the American Heart Association 2020;9(22):e018686. DOI: https://doi.org/10.1161/JAHA.120.018686
- Greenberg PE, Fournier AA, Sisitsky T, Simes M, Berman R, Koenigsberg SH, et al., The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics 2021;39(6):653-65. DOI: https://doi.org/10.1007/s40273-021-01019-4
- Who D. Other common mental disorders: global health estimates. World Health Organization, Geneva. 2017.
- Mathers CD and Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine 2006;3(11):e442. DOI: https://doi.org/10.1371/journal.pmed.0030442
- Feng HP, Chien WC, Cheng WT, Chung CH, Cheng SM, Tzeng WC. Risk of anxiety and depressive disorders in patients with myocardial infarction: A nationwide population-based cohort study. Medicine 2016;95(34):e4464. DOI: https://doi.org/10.1097/MD.0000000000004464
- Feng L, Li L, Liu W, Yang J, Wang Q, Shi L, et al., Prevalence of depression in myocardial infarction: a PRISMA-compliant meta-analysis. Medicine 2019;98(8):e14596. DOI: https://doi.org/10.1097/MD.0000000000014596
- Hosseini SH, Ghaemian A, Mehdizadeh E, Ashraf H. Contribution of depression and anxiety to impaired quality of life in survivors of myocardial infarction. International journal of psychiatry in clinical practice 2014;18(3):175-181. DOI: https://doi.org/10.3109/13651501.2014.940049
- Van Melle JP, De Jonge P, Spijkerman TA, Tijssen J, Ormel J, Van Veldhuisen, DJ, et al., Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosomatic medicine 2004;66(6):814-822. DOI: https://doi.org/10.3109/13651501.2014.940049
- Heron, M., 2021. Deaths: leading causes for 2019. DOI: https://dx.doi.org/10.15620/cdc:107021
- Celano CM, Huffman JC. Depression and cardiac disease: a review. Cardiology in review 2011;19(3):130-142. DOI: https://doi.org/10.1097/CRD.0b013e31820e8106.
- Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Journal of the American college of Cardiology 2006 17;48(8):1527-1537.
- Jee YH, Chang H, Jung KJ, Jee SH. Cohort study on the effects of depression on atherosclerotic cardiovascular disease risk in Korea. BMJ open 2019;9(6):e026913. DOI: https://doi.org/10.1136/bmjopen-2018-026913
- May HT, Horne BD, Knight S, Knowlton KU, Bair TL, Lappé DL, et al., The association of depression at any time to the risk of death following coronary artery disease diagnosis. European Heart Journal-Quality of Care and Clinical Outcomes 2017;3(4):296-302. DOI: https://doi.org/10.1093/ehjqcco/qcx017
- Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al., Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 2014;129(12):1350-1369. DOI: https://doi.org/10.1161/CIR.0000000000000019
- Geulayov G, Novikov I, Dankner D, Dankner R. Symptoms of depression and anxiety and 11-year all-cause mortality in men and women undergoing coronary artery bypass graft (CABG) surgery. Journal of psychosomatic research 2018;105:106-114. DOI: https://doi.org/10.1016/j.jpsychores.2017.11.017
- Lange HW, Herrmann-Lingen C. Depressive symptoms predict recurrence of atrial fibrillation after cardioversion. Journal of Psychosomatic Research 2007;63(5):509-513. DOI: https://doi.org/10.1016/j.jpsychores.2007.07.010
- Seligman F, Nemeroff CB. The interface of depression and cardiovascular disease: therapeutic implications. Annals of the New York Academy of Sciences 2015;1345(1):25-35. DOI: https://doi.org/10.1111/nyas.12738
- Smolderen KG, Buchanan DM, Gosch K, Whooley M, Chan PS, Vaccarino V, Parashar S, Shah AJ, Ho PM, Spertus JA. Depression treatment and 1-year mortality after acute myocardial infarction: insights from the TRIUMPH registry (Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status). Circulation 2017;135(18):1681-1689. DOI: https://doi.org/10.1161/CIRCULATIONAHA.116.025140
- Dhar AK, Barton DA. Depression and the link with cardiovascular disease. Frontiers in psychiatry 2016;21(7):33. DOI: https://doi.org/10.3389/fpsyt.2016.00033
- Schlaich MP, Kaye DM, Lambert E, Sommerville M, Socratous F, Esler MD. Relation between cardiac sympathetic activity and hypertensive left ventricular hypertrophy. Circulation 2003;108(5):560-565. DOI: https://doi.org/10.1161/01.CIR.0000081775.72651.B6
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosomatic medicine. 2004;66(3):305-315.
- Wilkowska A, Rynkiewicz A, Wdowczyk J, Landowski J. Morning and afternoon serum cortisol level in patients with post-myocardial infarction depression. Cardiology Journal. 2019;26(5):550-554. DOI: https://doi.org/10.5603/CJ.a2017.0123
- Elhwuegi AS. Central monoamines and their role in major d Murphy B, Le Grande M, Alvarenga M, Worcester M, Jackson A. Anxiety and depression after a cardiac event: prevalence and predictors. Frontiers in psychology 2020;10:3010. DOI: https://doi.org/10.3389/fpsyg.2019.03010
- Progress in Neuro-Psychopharmacology and Biological Psychiatry 2004;28(3):435-451. DOI: https://doi.org/10.1016/j.pnpbp.2003.11.018
- Acoba EF. Social support and mental health: the mediating role of perceived stress. Frontiers in Psychology 2024;21;15:1330720. DOI: https://doi.org/10.3389/fpsyg.2024.1330720
- Myers V, Gerber Y, Benyamini Y, Goldbourt U, Drory Y. Post-myocardial infarction depression: increased hospital admissions and reduced adoption of secondary prevention measures—a longitudinal study. Journal of Psychosomatic Research 2012;72(1):5-10. DOI: https://doi.org/10.1016/j.jpsychores.2011.09.009
- Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychology, health & medicine 2013;18(6):627-644. DOI: https://doi.org/10.1080/13548506.2012.749355
- Larsen KK, Vestergaard M, Søndergaard J, Christensen B. Screening for depression in patients with myocardial infarction by general practitioners. European journal of preventive cardiology 2013;20(5):800-806. DOI: https://doi.org/10.1177/2047487312444994
- Lu Y, Wang Z, Georgakis MK, Lin H, Zheng L. Genetic liability to depression and risk of coronary artery disease, myocardial infarction, and other cardiovascular outcomes. Journal of the American Heart Association 2021;10(1):e017986. DOI: https://doi.org/10.1161/JAHA.120.01798
- Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. American Journal of Psychiatry 2007;164(9):1379-1384. DOI: https://doi.org/10.1176/appi.ajp.2007.06101617
- Schins A, Honig A, Crijns H, Baur L, Hamulyák K. Increased coronary events in depressed cardiovascular patients: 5-HT2A receptor as missing link?. Psychosomatic medicine 2003;65(5):729-737. DOI: https://doi.org/10.1097/01.PSY.0000088596.42029.10
- Nakatani D, Sato H, Sakata Y, Shiotani I, Kinjo K, Mizuno H, et al. Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. American heart journal 2005;150(4):652-658. DOI: https://doi.org/10.1016/j.ahj.2005.03.062
- Jha MK, Qamar A, Vaduganathan M, Charney DS, Murrough JW. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. Journal of the American College of Cardiology 2019;73(14):1827-1845.
- Guck TP, Kavan MG, Elsasser GN, Barone EJ. Assessment and treatment of depression following myocardial infarction. American Family Physician 2001;64(4):641-648.
- Taylor D, Meader N, Bird V, Pilling S, Creed F, Goldberg D. Pharmacological interventions for people with depression and chronic physical health problems: systematic review and meta-analyses of safety and efficacy. The British Journal of Psychiatry 2011;198(3):179-188. DOI: https://doi.org/10.1192/bjp.bp.110.077610
![]() This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution‑Non-Commercial‑ShareAlike 4.0 International License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as appropriate credit is given, and the new creations are licensed under the identical terms.
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution‑Non-Commercial‑ShareAlike 4.0 International License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as appropriate credit is given, and the new creations are licensed under the identical terms.
